A Guide to NDIS Physiotherapy in the Community
Have you heard of NDIS physiotherapy in the community but are not sure whether it would be beneficial for you or you client to engage in it? Physiotherapists can assist with a broad range of conditions for people of any age and focus on how to best achieve a participant’s goals by improving their movement. Our clients achieve great outcomes when engaging in NDIS physiotherapy in the community, so this service may also be beneficial for you and your clients.
To answer some common questions about NDIS physiotherapy in the community and help you decide whether you should engage in National 360’s physiotherapy services to assist in achieving your goals or the goals of your client, watch the video below, or scroll down further read the answers to the common questions below.
What does a Physiotherapist do?
First, a physiotherapist would go in and assess. From our assessment we would make a diagnosis. With a client under the NDIS, the diagnosis has already been made, so diagnosis might be that we are thinking about what are the client’s needs, their goals, and how am I going to get them from A to B? That’s where we make the plan, we put in our treatment or management plan, we review them to see how it is all going and what steps are they making to achieve these goals and we do that by reassessing – we’d go back around the cycle again, as depicted below. Physiotherapists are constantly assessing, reviewing, intervening, and working out what the client needs.

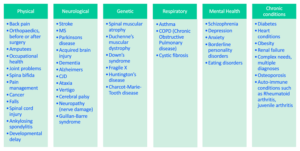
What conditions do Physiotherapists see?
Physiotherapists see a very broad range of conditions, so we thought it would be helpful to break it down into categories. We’ve got the Physical, Neurological, Genetic, Respiratory, Mental Health and Chronic Conditions categories. You can see (in table below) there are lots of conditions and diagnoses that fall under each category, and these all cover a range of ages as well. Physical, Neurological and Genetic we might be seeing children, adults, aged care – same thing with mental health as well – we might cover a range of ages that we are seeing.
There is a huge range of conditions that we see, but one person with a condition is not necessarily going to be the same as the next person with the condition, so we are not treating by condition, we’re treating what the goals are, and the needs of the client. That’s really the main point for us, to assess clients individually, and work out an individual plan, work out their individual goals, and we’re still obviously considering their diagnoses, but we are trying to treat each client as an individual.
Why should I [or my client] engage in NDIS physiotherapy in the community?
Physiotherapists are thinking about the goals, so what we can achieve with that person – Are we looking to improve their mobility? Improve some functional tasks? Is it exercise tolerance and fitness? For example, this person can’t walk 10-minutes at the moment, but they want to be able to walk to the park or walk to the coffee shop that is 30-minutes away. Are we thinking about falls prevention? Does the client have balance issues? Is it a return-to-work issue? Is there therapy involved for play or are we looking to improve fine motor control or gross motor skills? A physiotherapist is really thinking about the person’s needs, their goals, and how NDIS physiotherapy in the community can bridge the gap.
Can Physiotherapists prescribe Assistive Technology (AT) Equipment?
Physiotherapists have got specific skills related to Assistive Technology (AT) prescription, either that we can provide equipment independently ourselves from the assessment that we’ve done, or it may be that we need to liaise with and involve equipment specialists, or it may be that we need to liaise with other therapists as well and do a joint assessment and collaborate together to get the best outcome for the patient. Our aim is always to improve the person’s function and activity, so ultimately, we are trying to work on improving the person’s participation in their social life and get them involved in their community.
How can a Support Coordinator describe the difference between how a Physiotherapists and an Occupational Therapist assesses mobility to their participant or client?
Physiotherapists are going to be looking very much at the physical aspect of how a participant/client moves, and where we can improve their movement. The physical side of things is really a physiotherapist’s bread and butter, that’s our training and we’ve got those diagnostic skills physically to be able to look at somebody that, for example, may be hitching their hip up to swing the leg through and assess – is that an issue with the hip, is that an issue with the back, is that an issue with the knee, or is that an issue with the foot? We can hone in on and analyse exactly what is going on and what could be causing that.
The physio is going to be looking more around the physical side of things, and the Occupational Therapist (OT) may be looking more from a functional level, so it comes back to that both professions can work well together, but in terms of somebody’s mobility, physios are analysing somebody’s ability to move, and that is really where our strengths lie. The physio looks at the client’s actual body and body parts and how they move, whereas the OT looks at what the client can do as a function. Physios look at the body – OT is looking at the task.
What’s the difference between a Physiotherapist and an Exercise Physiologist?
This question we get asked a lot, because it seems that both physiotherapists and exercise physiologists (EP) are the same profession, but we’re not the same. There is a lot of overlap between a physio and an exercise physiologist. Both of us are involved in exercise prescription, but, the main difference is that an EP cannot diagnose a movement problem, they need to be given the diagnosis itself then they will be able to prescribe an exercise program.
For example, in the case of a stroke patient, the EP can look at the stroke patient and how this person walks and see that they might need some strengthening in the legs or arms, and then they will give a very generic strengthening program for the legs or the arms, but they wouldn’t be able to analyse why this person is walking a bit strange, or they they’re lopsided. Whereas the physio can analyse why this person has decreased balance, or why their walking pattern is a bit strange and are able to target and correct that movement pattern to improve their walking pattern.
The physio is more targeted and more specific to the joint or the actual movement itself whereas the EP would be targeting a more general and broad exercise program.
Contact National 360 about NDIS Physiotherapy in the community today!
For more information about why NDIS physiotherapy in the community in beneficial, and National 360’s Physiotherapy services, click here.
For you’d like to engage in NDIS Physiotherapy in the community with National 360 and would like to complete our online referral form, click here, or fill our out details below.



